Our Current Research
KRAS
Mechanisms of KRAS G12C inhibitor resistance
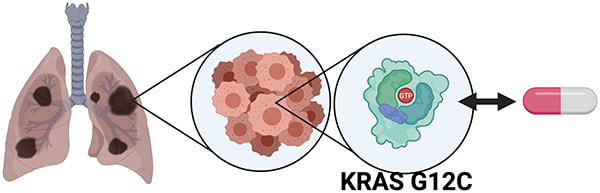
KRAS (Kirsten Rat Sarcoma Viral Homologue) is the most frequently mutated oncogene in human cancer. Glycine to cysteine mutations in codon 12 of KRAS are highly prevalent, accounting for 14%, 4%, and 2% of NSCLC, colorectal and pancreatic cancer cases. KRAS was considered "undruggable" until recent FDA-approval of two structurally different, highly selective, covalent inhibitors, sotorasib and adagrasib, for the treatment of NSCLC patients harboring oncogenic KRASG12C mutations.
Despite efficacious initial responses to sotorasib and adagrasib in patients, cases of innate and acquired drug resistance quickly emerge after treatment. Thus, alternative therapeutic approaches are needed to prevent or overcome resistance. Several lines of investigation suggest multifaceted mechanisms of drug resistance: tumors can compensate drug inhibition with the amplification of KRAS, acquire new mutations in the KRAS oncogene, or find alternative pathways of activation. Moreover, it is believed that intracellular heterogeneity or intercellular variability is the primary cause of resistance to KRASG12C inhibitors. The complexity of drug resistance ranges from the acquisition of secondary on-target mutations in KRAS, affecting the inhibitor-binding pocket of off-target mutations downstream of KRAS. Non-genetic mechanisms of drug resistance such as histologic transformations in NSCLC or the rewiring of the proteostasis network by drug tolerant cells to escape drug inhibition have also been observed.
Overcoming the heterogeneous, resistant cell populations requires combinatorial drug treatments that inhibit both the original the KRAS mutation as well as the alternatives. Consequently, ongoing clinical trials to improve the efficiency of sotorasib and adagrasib include combining the drugs with EGFR, MET or SHP2 inhibitors in order to block the activation of proliferative signaling. Although it is expected that these drug combinations will provide better tumor responses and progression-free survival, these combination treatments often face dose-limiting toxicities and bring about new pathways of resistance. We are exploring novel methods to improve the efficacy of small molecule KRAS G12C as well as KRAS G12D inhibitors.
Despite efficacious initial responses to sotorasib and adagrasib in patients, cases of innate and acquired drug resistance quickly emerge after treatment. Thus, alternative therapeutic approaches are needed to prevent or overcome resistance. Several lines of investigation suggest multifaceted mechanisms of drug resistance: tumors can compensate drug inhibition with the amplification of KRAS, acquire new mutations in the KRAS oncogene, or find alternative pathways of activation. Moreover, it is believed that intracellular heterogeneity or intercellular variability is the primary cause of resistance to KRASG12C inhibitors. The complexity of drug resistance ranges from the acquisition of secondary on-target mutations in KRAS, affecting the inhibitor-binding pocket of off-target mutations downstream of KRAS. Non-genetic mechanisms of drug resistance such as histologic transformations in NSCLC or the rewiring of the proteostasis network by drug tolerant cells to escape drug inhibition have also been observed.
Overcoming the heterogeneous, resistant cell populations requires combinatorial drug treatments that inhibit both the original the KRAS mutation as well as the alternatives. Consequently, ongoing clinical trials to improve the efficiency of sotorasib and adagrasib include combining the drugs with EGFR, MET or SHP2 inhibitors in order to block the activation of proliferative signaling. Although it is expected that these drug combinations will provide better tumor responses and progression-free survival, these combination treatments often face dose-limiting toxicities and bring about new pathways of resistance. We are exploring novel methods to improve the efficacy of small molecule KRAS G12C as well as KRAS G12D inhibitors.